Connect With Us
Blog
Items filtered by date: October 2024
Foot Arthritis and Finding Relief

Foot arthritis encompasses several conditions that can cause pain and inflammation in the joints. Rheumatoid arthritis is an autoimmune disorder that leads to chronic inflammation, often affecting multiple joints in the feet. Psoriatic arthritis, associated with psoriasis, can also impact the toes and joints, causing swelling and discomfort. Osteoarthritis, a degenerative joint disease, results from wear and tear over time, leading to stiffness and pain. Gout, characterized by sudden and severe pain, occurs when uric acid crystals accumulate in the joints, frequently affecting the big toe. Finding relief from foot arthritis involves a combination of strategies. Resting and elevating the feet can help reduce swelling. Wearing supportive footwear and engaging in low-impact exercises can improve mobility and enhance overall foot health. If you have arthritic foot symptoms, it is suggested that you consult a podiatrist who can offer you effective relief options.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact James Torhorst, DPM from Torhorst Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Waupaca and Stevens Point, WI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
It's Time for Beautiful Feet
How to Manage Bunions

A bunion is a bony bump that forms at the base of the big toe, where it meets the long bone of the foot. Bunions develop when the big toe pushes towards the second toe, causing the joint at the base of the big toe to protrude. This misalignment is often made worse by wearing tight or ill-fitting shoes, particularly those with high heels or a narrow toe box. Symptoms of bunions include pain, swelling, and redness surrounding the affected joint, and difficulty finding comfortable footwear. Over time, the misalignment can worsen, making daily activities uncomfortable. Treatment for bunions focuses on alleviating pain and preventing further progression. A podiatrist can discuss options that may include wearing wider, more supportive shoes, using orthotic devices to correct foot alignment, and performing exercises to improve joint mobility. In persistent cases, surgery may be considered. If you have developed a bunion, it is suggested you schedule an appointment with a podiatrist for a treatment plan.
If you are suffering from bunions, contact James Torhorst, DPM of Torhorst Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Waupaca and Stevens Point, WI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Managing Cuts on the Bottom of the Feet

Managing cuts on the bottom of the feet, which requires prompt and careful attention to prevent infection and promote healing, is often done by a podiatrist. This type of doctor will start by cleaning the wound thoroughly with mild soap and water to remove any debris and reduce the risk of infection. This is generally followed by gently patting the area dry with a clean cloth or gauze. The doctor will then apply an antiseptic to the cut to further disinfect the area, and cover the wound with a sterile adhesive bandage or dressing to protect it from dirt and friction. The dressing will be secure but not too tight, allowing for comfort and breathability. Regularly changing the dressing and monitoring the cut for signs of infection, such as increased redness, swelling, or discharge will be recommended. If you have a cut on the bottom of your foot, it is suggested that you schedule an appointment with a podiatrist who can offer you effective treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with James Torhorst, DPM from Torhorst Foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Waupaca and Stevens Point, WI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Manage an Ingrown Toenail

Ingrown toenails occur when the edge of a toenail grows into the surrounding skin, causing pain, swelling, and sometimes infection. The big toe is most commonly affected. Causes include improper nail trimming, wearing tight or ill-fitting shoes, injury to the toenail, or genetic predisposition. Symptoms of an ingrown toenail include redness, swelling, pain, and tenderness along the side of the nail. If left untreated, the area can become infected, leading to pus, warmth, and increased pain. If you have toe pain and notice symptoms of an ingrown toenail, it is suggested that you visit a podiatrist who can guide you toward effective treatment, which may include partial nail removal.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact James Torhorst, DPM of Torhorst Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our offices located in Waupaca and Stevens Point, WI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Why Do Some Children Get Sever’s Disease?
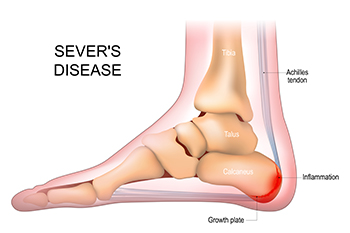
Sever's disease, also known as calcaneal apophysitis, is an overuse injury that affects the growth plate in the heel of growing children and adolescents, usually between the ages of eight and 15. It occurs when repetitive stress or pressure on the heel bone, often from sports or physical activities, causes inflammation and pain in the heel. Sever's disease is common in children who are physically active and going through growth spurts, as the bones grow faster than the muscles and tendons, leading to increased tension on the heel. It manifests as heel pain, swelling, and tenderness, particularly during or after physical activity. Treatment focuses on reducing activity levels and wearing supportive footwear or orthotics. Most children outgrow the condition once their bones stop growing. If your child has heel pain that is persistent, it is suggested that an appointment be made with a podiatrist for a proper diagnosis and treatment to alleviate pain.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see James Torhorst, DPM from Torhorst Foot and Ankle. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Waupaca and Stevens Point, WI . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.

